Preemptive Fraud, Waste and Abuse Defense for Home Health & Personal Care Services
Ensuring integrity and accuracy in specialized, high-volume healthcare areas
Total fraud, waste and abuse identified for our clients
$600 Million
Home health & Personal Care
$330 Million
Pharmacy
$55 Million
Therapy
$16 Million
Dental
$12 Million
Ambulance
$6 Million
Vision
$4 Million
Workers' Compensation
Ready To Deploy Configurable Edits
List of configurable edits to satisfy in-house policies, regulatory changes and unique contracts
- Provider exclusion list
- 24 hour rule
- Impossible day
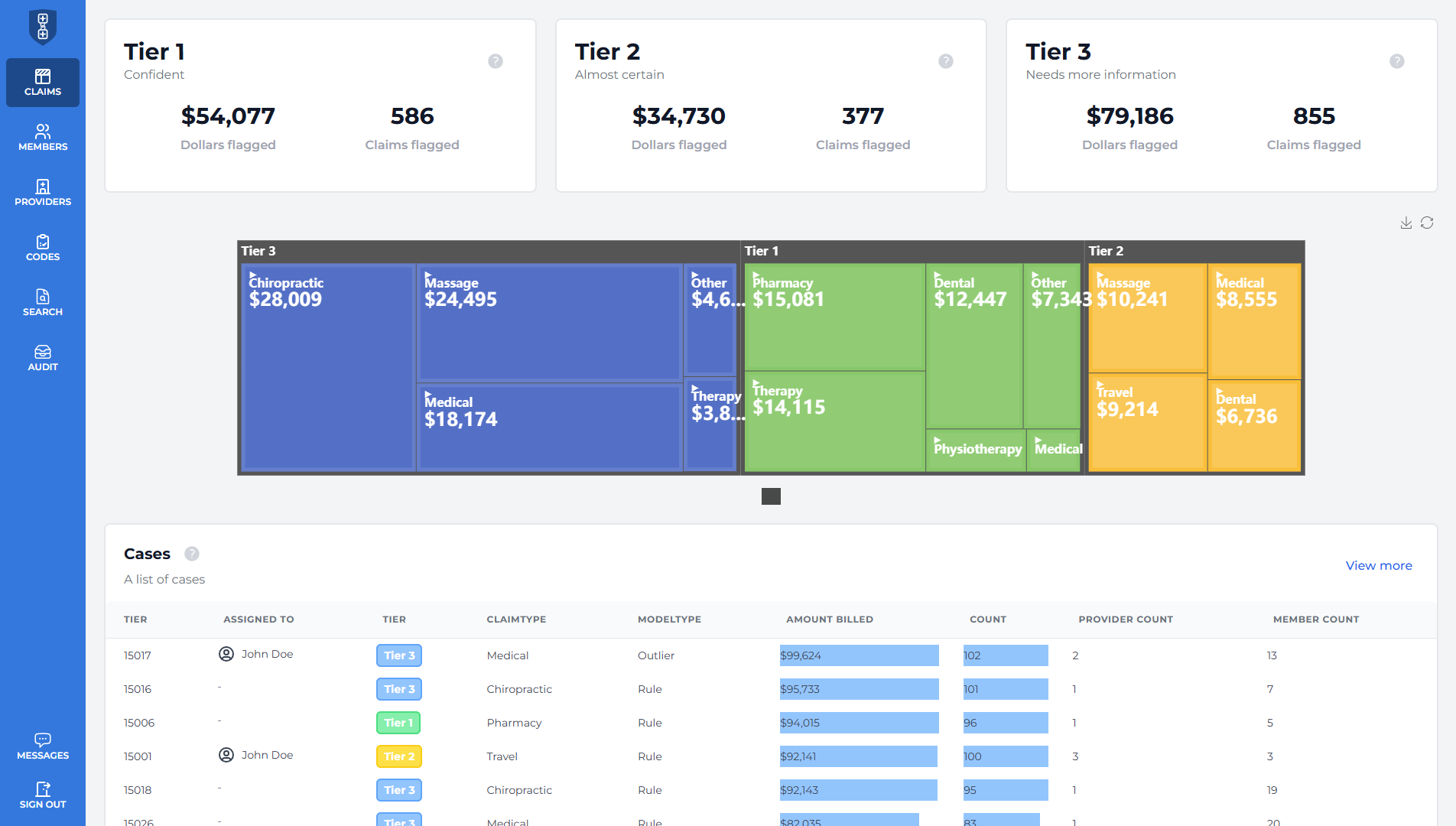
Real Time Payor Dashboard For Analytics
Precise pre-pay claim flagging using our AI models and analytics visible on a dashboard
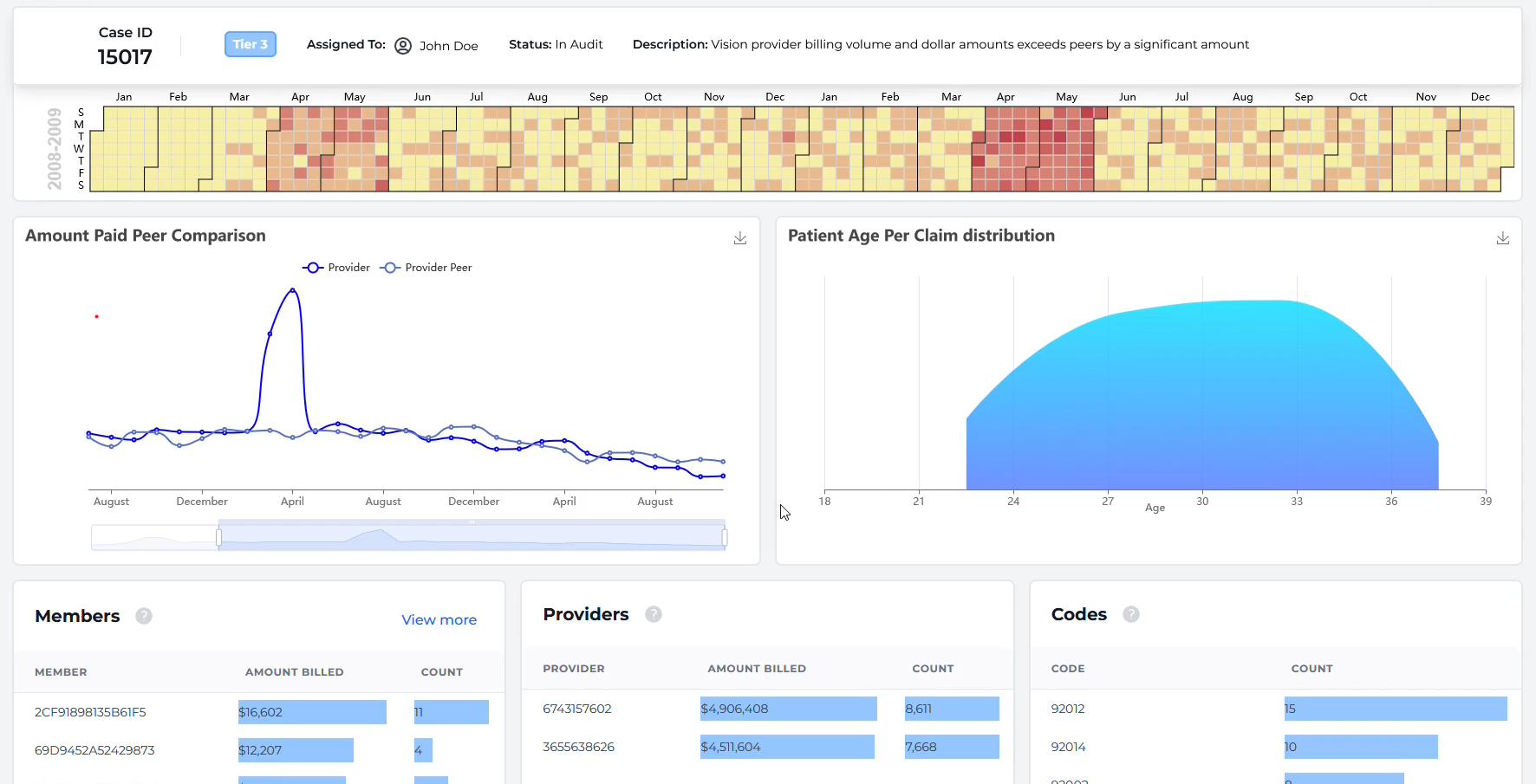
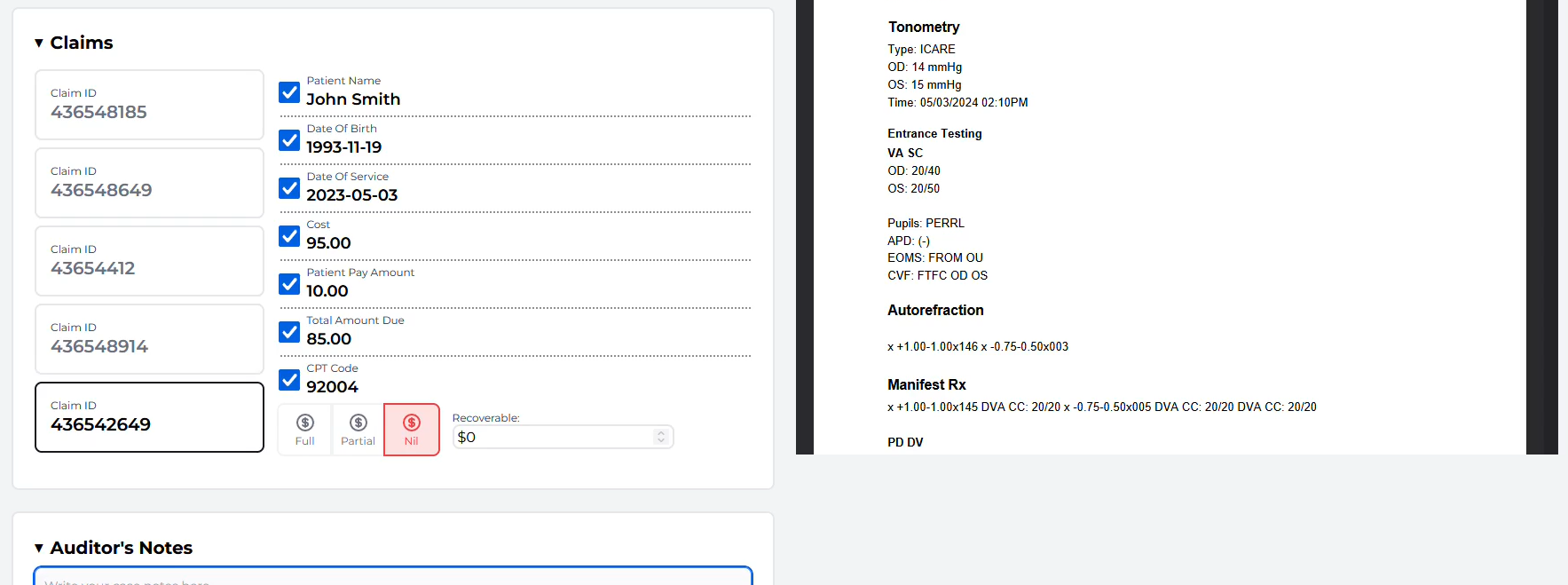
AI Enhanced Expert Claim Audit
Results up to 70% faster with claim review by expert clinicians, coders and subject matter experts using AI to deliver results
Secure by default
HITRUST, HIPAA and PIPEDA compliant
Low Cost, High Dollar Health Services Are Our Speciality
Handle all types of supplemental health claims
- Pharmacy - Dental - Optical - Home Health - Personal Care - Therapy - Ambulance -
Workers' Compensation - DME - Chiropractic
- Pharmacy - Dental - Optical - Home Health - Personal Care - Therapy - Ambulance -
Workers' Compensation - DME - Chiropractic
US and Canada Claims Supported
Analyze claims with codes (such as DIN, NDC, CPT, OHIP, etc) from both Canada and US
Contact our team to explore your saving opportunities
Have your questions answered and get acquainted with our products.
- Learn how to increase payment accuracy and lower healthcare expenditure
- Explore use cases for your payment integrity team
- Get any questions answered about our products
Email us at sales@metadigital.tech or reach out on LinkedIn
Payers have identified $1.8 billion in
fraud, waste and abuse using MetaDigital.